 Minor gastrointestinal problems, known in medical terms as functional gastrointestinal disorders (FGIDs), occur very frequently during the first months of life. In most cases the infant does not have an underlying medical problem and grows and develops normally. FGID symptoms can be easily remedied by a special infant formula containing carob bean gum and GOS in an anti-reflux or AR formula that offers thickening and prebiotic properties. It is classified as a food for special medical purposes (FSMP) especially for infants.
Minor gastrointestinal problems, known in medical terms as functional gastrointestinal disorders (FGIDs), occur very frequently during the first months of life. In most cases the infant does not have an underlying medical problem and grows and develops normally. FGID symptoms can be easily remedied by a special infant formula containing carob bean gum and GOS in an anti-reflux or AR formula that offers thickening and prebiotic properties. It is classified as a food for special medical purposes (FSMP) especially for infants.
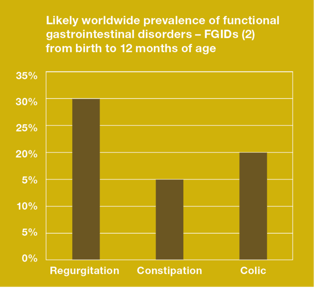
Regurgitation, constipation and colic are the most common functional gastrointestinal disorders. They often cause parental anxiety and avoidable feeding changes (1, 2, 3). Studies prove that 55% of infants under six months of age suffer from gastrointestinal discomfort and 39% of these infants experience a combination of symptoms.
Regurgitation
Almost all infants bring up small amounts of milk after a feed, whether they are breast fed or bottle fed. Reflux, regurgitation, posseting or spitting up is common in infants; as long as the baby is otherwise happy, healthy and gaining weight, there’s generally no cause for concern. Daily regurgitation has a prevalence of about 87% at two months of age (4). These infants are referred to as ‘happy spitters’ – a temporary, non-serious problem that usually gets better as the baby’s digestive system matures.
Non-closure of the protective one-way valve at the upper end of the stomach (known as the lower esophageal sphincter or LES) is responsible for regurgitation. In infants, this LES is not yet fully mature, which allows stomach contents to flow backward via the oesophagus (the connecting tube) to the mouth. During the first year of life, the sphincter action gradually gets stronger and the chance of regurgitation decreases. The terms reflux and regurgitation are often used interchangeably. In medical terms, however, this condition is called Gastro-Oesophageal Reflux (GOR). GOR can also be caused by the method of feeding. An excessive amount of food in the stomach or swallowing of air, caused by excessive drinking, can lead to increased stomach pressure. This can result in cramps or backflow of food in the stomach. GOR is common in young infants because their gastrointestinal tract is still developing.
"The reduction in episodes and volume of regurgitation is a welcome improvement in quality of life for infants and caregivers."
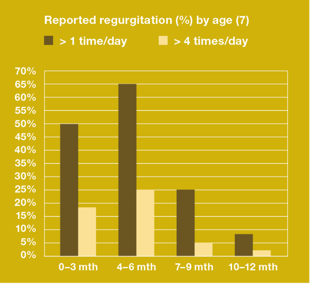
Complaints of regurgitation are known to peak at the age of three to four months. During this period they occur in 50% to 70% of infants. Regurgitation resolves spontaneously in most healthy infants by 12 to 14 months (5, 6). Parents view the symptom as a problem more often than medical intervention is given. About 25% of the parents seek medical help because of infant regurgitation (2, 5).
Regurgitation occurs as often in breast-fed as bottle-fed children. Because it frequently leads to parental anxiety, reassuring the parents and offering practical advice on the correct drinking technique and the distribution of feeds over the day (offer small amounts regularly) can help. Several studies show that in formula-fed infants, an AR formula decreases the frequency and volume of regurgitation (9). AR formula contains carob bean gum, which thickens the formula and subsequently reduces regurgitation, along with added prebiotics (GOS) – making it safe and effective.
Hard stools and/or associated cramps
Like regurgitation, hard stools (mild constipation) and cramps (colics) are a common complaint in infants.
Hard stools or mild constipation are defined as difficult defaecation, lasting for two or more weeks. It occurs in 15% of the infants younger than 12 months. In infants younger than four months, the type of feeding has a key role in the stool pattern. Every infant has its own bowel pattern; the baby’s individual pattern depends on what it eats and drinks, how active it is, and how quickly it digests food. It seldom occurs with breast feeding and is more common with forumla feeding (8).
Any extreme changes affecting the infant may cause a decreased frequency of stools or may harden stools. Firm or hard stools are often seen when changing from breast milk to an infant formula or after the introduction of solid food. It takes some time for the infant’s bowel to get used to new food. Another cause can be illness with fever or a reduced food/fluid intake, which produces a disturbed fluid balance. As with regurgitation, the first step in treatment is always parental education. It should be pointed out that hard stools are a common and non-dangerous problem in infancy that usually disappears. For bottle feeding, it is important that the formula is prepared correctly (right amount of powder and water) and the daily fluid intake is appropriate.
Hard stools may occur in combination with colic. Colic and colic pains or cramps are characterised by stomach pain and often accompanied by excessive crying. Infants usually communicate and express themselves by crying. By the time parents visit the doctor with their crying child, they are often anxious, frustrated, and sleep-deprived. The crying and fussiness can last for hours at a stretch, followed by periods when the baby acts and seems perfectly comfortable. The crying episodes tend to increase at six weeks of age and occur mostly in the late afternoon. The cause of infantile colic is generally unknown but there is increased evidence that it is related to a food allergy, an altered gastro-intestinal function, microflora imbalance, GOR or cow’s milk allergy (9). Colic affects 20% of babies worldwide and impacts breast-fed and bottle-fed infants equally (2, 8). The condition usually resolves spontaneously by the age of about four months.
Carob bean gum: safe & effective
In addition to thickening properties that reduce regurgitation, AR formula with carob bean gum also has prebiotic properties that have a relieving effect on hard stools and/or associated colic. Added galacto-oligosaccharides (GOS) are prebiotics in the form of a fermentable fibre that stimulates the growth of ‘good bacteria’ (bifidobacteria and lactobacilli) in the gut. This results in an increased stool volume and softness. In general, it creates a better gut motility. That’s why this formula is also well suited to infants who suffer from hard stools and/or associated cramps.
Further information
- Short article "Regurgitation Olivias Story"
- Overview "Carob bean gum"
- Article "Prebiotics in infant formula – part 1"
- Article "Prebiotics in follow-on foods – part 2"
- Overview "Specialist formula"
Sources
1) Iacono G., et al. The Pediatric Study Group on Gastrointestinal Symptoms in Infancy. Gastrointestinal symptoms in infancy: a population-based prospective study. Dig Liver Dis 2005;37:432-438.
2) Vandenplas Y., et al. Prevalence and health outcomes of functional gastrointestinal symptoms in infants from birth to 12 months of age. J Pediatr Gastroenterol Nutr 2015;61:5:531-37.
3) Zeevenhooven J., et al. The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers. Pediatr Gastroenterol Hepatol Nutr 2017;20(1):1-13.
4) Vandenplas Y., et al. Practical algorithms for managing common gastrointestinal symptoms in infants. Nutrition 2013;29(1):184-194.
5) Dupont C., et al. Efficacy and tolerance of a new anti-regurgitation formula. Pediatr Gastroenterol Hepatol Nutr 2016;19(2):104-109.
6) Vandenplas Y., et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr 2009;49(4):498-547.
7) Nelson S.P., et al. Prevalence of symptoms of gastro-esophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med; 1997;151: 569-572.
8) Vandenplas Y., et al. Updated algorithms for managing frequent gastro-intestinal symptoms in infants. Beneficial Microbes 2015;6(2):199-208.
9) Miranda, A. Early life stress and pain: an important link to functional bowel disorders. Pediatric Annals 2009;38:279-282.










Leave a comment